2023 Annual Clinical Assembly Poster Competition- Ophthalmology Entries

Niemann-Pick disease subtypes and ocular manifestations
Mark Shokralla, B.A. is a third-year medical student at William Carey University College of Osteopathic Medicine with a special interest in Ophthalmology.
Abstract
View Abstract
Summary
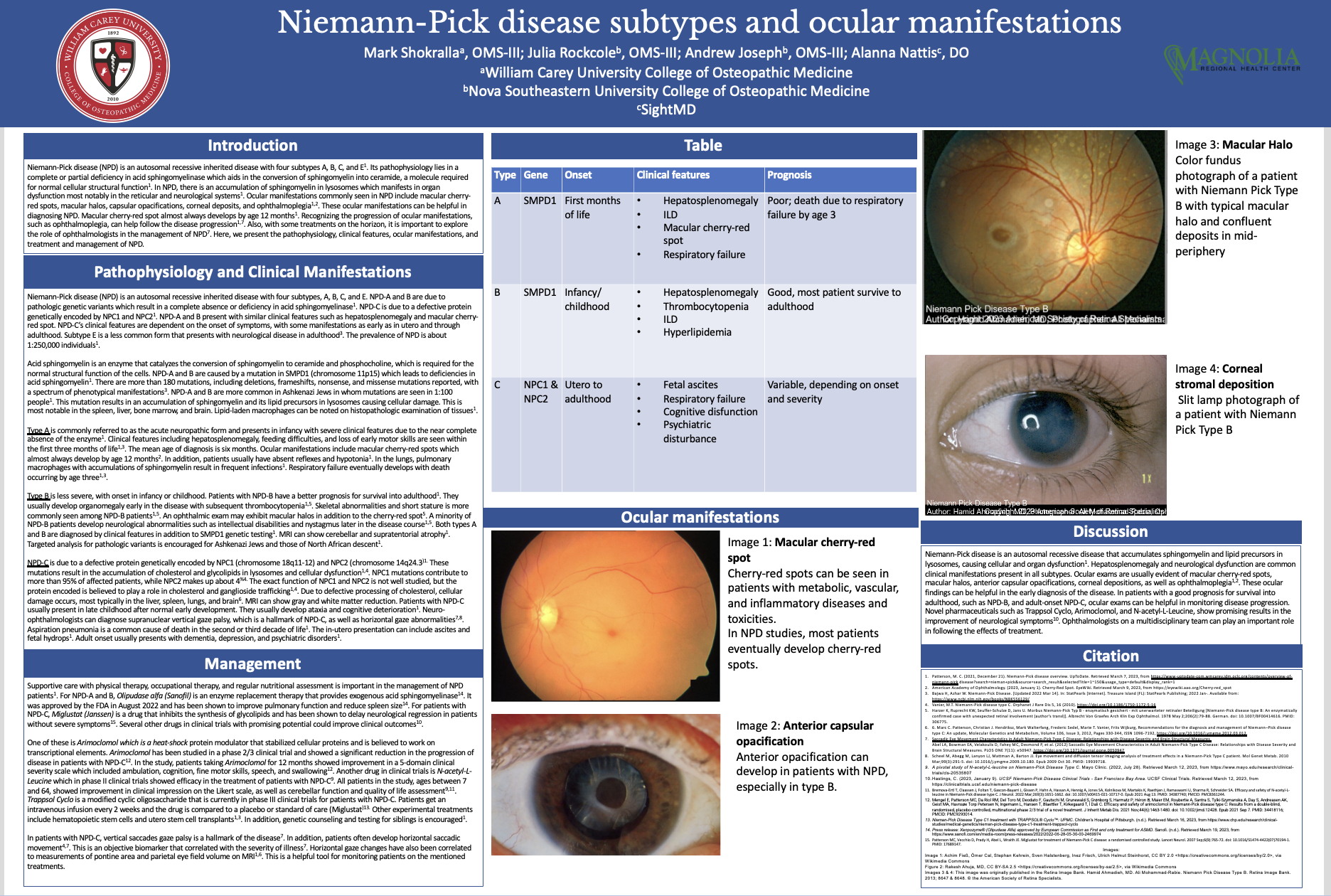
Niemann-Pick disease (NPD) is a rare autosomal recessive disease that results in the accumulation of sphingomyelin and lipid precursors in lysosomes causing cellular and organ dysfunction, most notably in the reticular and neurological systems. There are four subtypes of NPD: type A, B, C, and E, each with varying disease onset and presentation. Common ocular manifestations include macular cherry-red spots, macular halos, anterior capsular opacifications, corneal deposits, and ophthalmoplegias. As such, ophthalmologists can play a critical role in diagnosing Niemann-Pick disease and monitoring disease progression. Alongside frequent ophthalmology exams, current management includes supportive care, routine blood work, and monitoring/further workup of other non-neurologic manifestations. In addition, there have been some novel drug therapies for treating NPD. Olipudase alfa is an exogenous acid sphingomyelinase enzyme replacement therapy, recently approved by the FDA to treat NPD-A and B. Miglustat, which inhibits the synthesis of glycolipids, helps delay neurological regression in NPD-C patients with severe symptoms. Trappsol Cyclo, Arimoclomol, and N-acetyl-L-Leucine are other potential treatments that have shown promising results in recent clinical trials. This presentation serves to further outlines the pathophysiology, clinical manifestations, current management, and novel pharmaceuticals for the different subtypes of NPD.

Harris Ahmed DO, MPH
Nationwide Trends in Ophthalmic Trauma Related to Major Sports: An NEISS Study
Resident Physician at Loma Linda University Eye Institute (PGY-3). MPH from the University of Southern California. Current American Medical Association Ambassador. Former AOCOOHNS Resident and Fellow Chair - Ophthalmology
Abstract
View Abstract
Summary
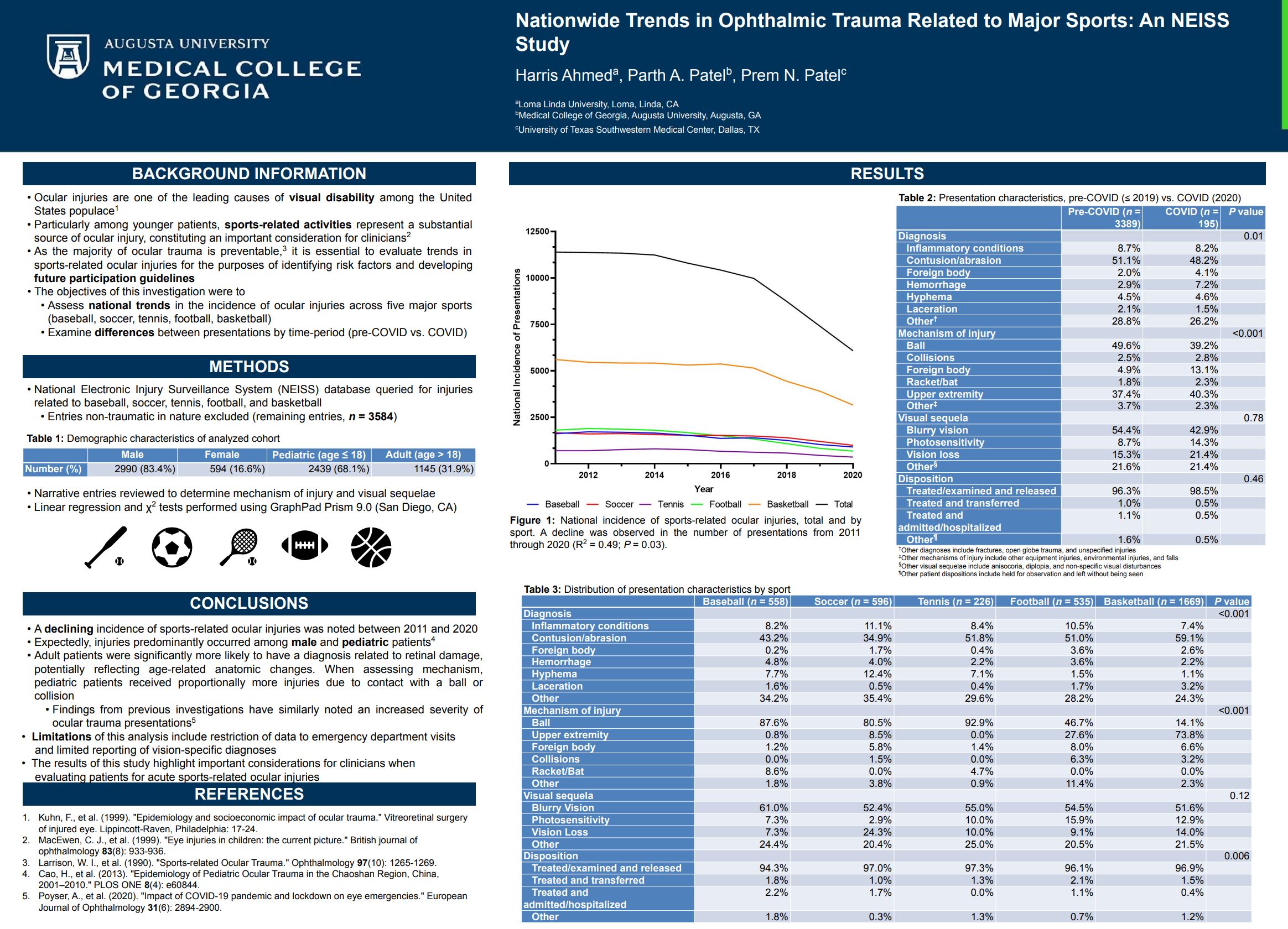
Our investigation demonstrated a decline in sports-related ocular injuries from 2011–2020, particularly after 2017. This trend may be partially explained by declining participation in youth sports (a phenomenon perpetuated by COVID-19) and regulation alterations to minimize contact. For example, widespread guidelines have been implemented to reduce full-contact drills in football.
Injuries predominantly occurred among pediatric and male patients, consistent with prior studies of sports-related ocular trauma. Adult patients were significantly more likely to have a diagnosis related to retinal damage, potentially reflecting age-related anatomic changes. When assessing mechanism, pediatric patients received proportionally more injuries due to contact with a ball or collision. Such differences are expected as children largely have poorer coordination, reflexes, and mechanical skills.8 Men were more likely to be injured from contact with another individual, a disparity that may originate from a greater inclination to engage in aggressive play. Alternatively, women could be predisposed to equipment injuries due to intrinsic (e.g., cellular response to injury) and extrinsic (e.g., resource allocation, differential training) factors. These factors may similarly account for differences in visual sequelae (i.e., photophobia).

Ibtisam Atamna OMS3
Diagnosis and Management of Diabetic Retinopathy
Ibtisam Sara Atamna is a third year medical student at Edward Via College of Osteopathic Medicine Carolinas campus.
Abstract
View Abstract
Summary
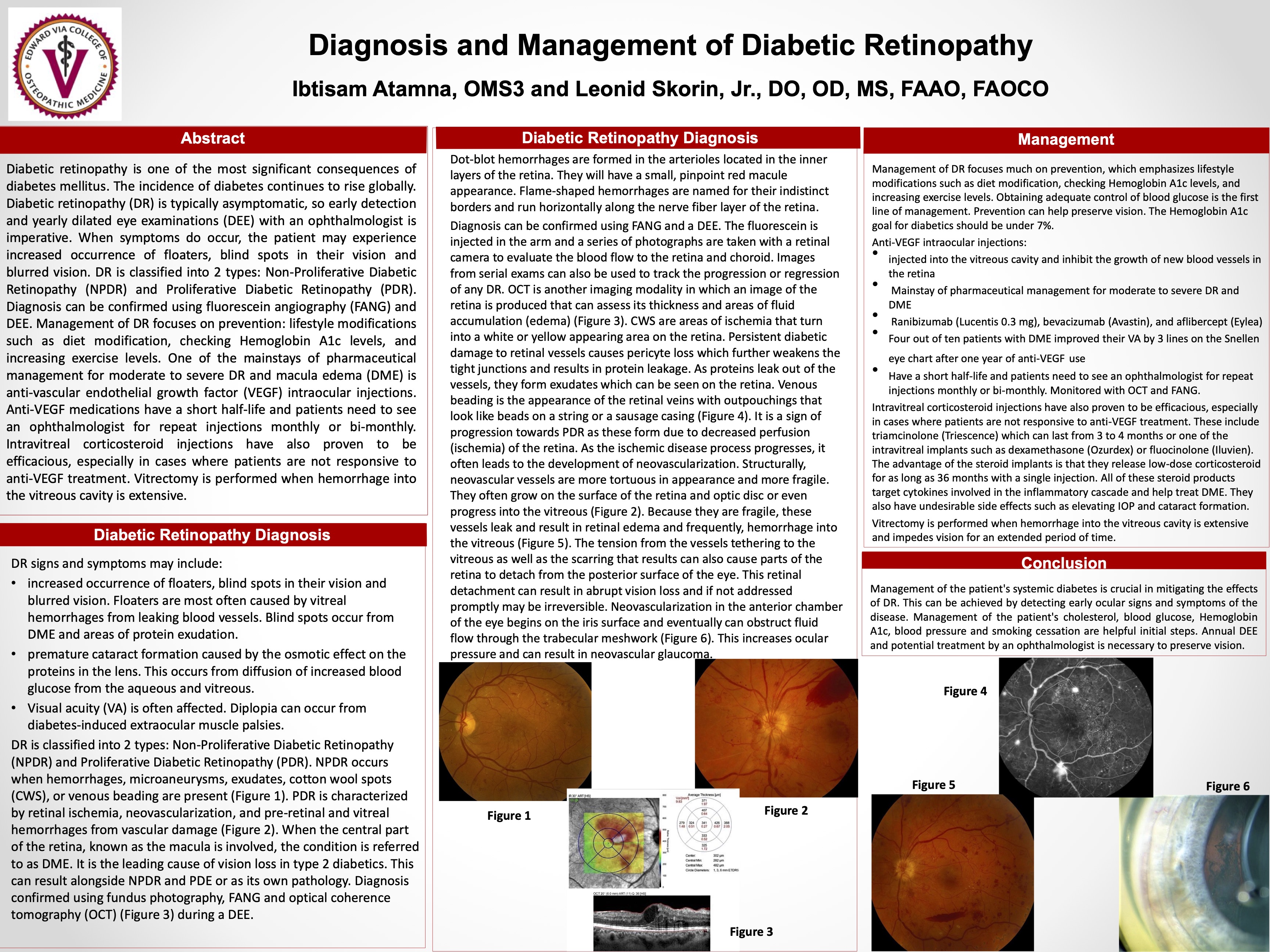
Diabetic retinopathy is one of the most significant consequences of diabetes mellitus. The incidence of diabetes continues to rise globally. Diabetic retinopathy (DR) is typically asymptomatic, so early detection and yearly dilated eye examinations (DEE) with an ophthalmologist is imperative. When symptoms do occur, the patient may experience increased occurrence of floaters, blind spots in their vision and blurred vision. DR is classified into 2 types: Non-Proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR). Diagnosis can be confirmed using fluorescein angiography (FANG) and DEE. Management of DR focuses on prevention: lifestyle modifications such as diet modification, checking Hemoglobin A1c levels, and increasing exercise levels. One of the mainstays of pharmaceutical management for moderate to severe DR and macula edema (DME) is anti-vascular endothelial growth factor (VEGF) intraocular injections. Anti-VEGF medications have a short half-life and patients need to see an ophthalmologist for repeat injections monthly or bi-monthly. Intravitreal corticosteroid injections have also proven to be efficacious, especially in cases where patients are not responsive to anti-VEGF treatment. Vitrectomy is performed when hemorrhage into the vitreous cavity is extensive.
Luke Barrick OMS3
Corneal Ulceration in the Setting of Pembrolizumab Treatment for Oropharyngeal Squamous Cell Carcinoma
Abstract
View Abstract
Summary
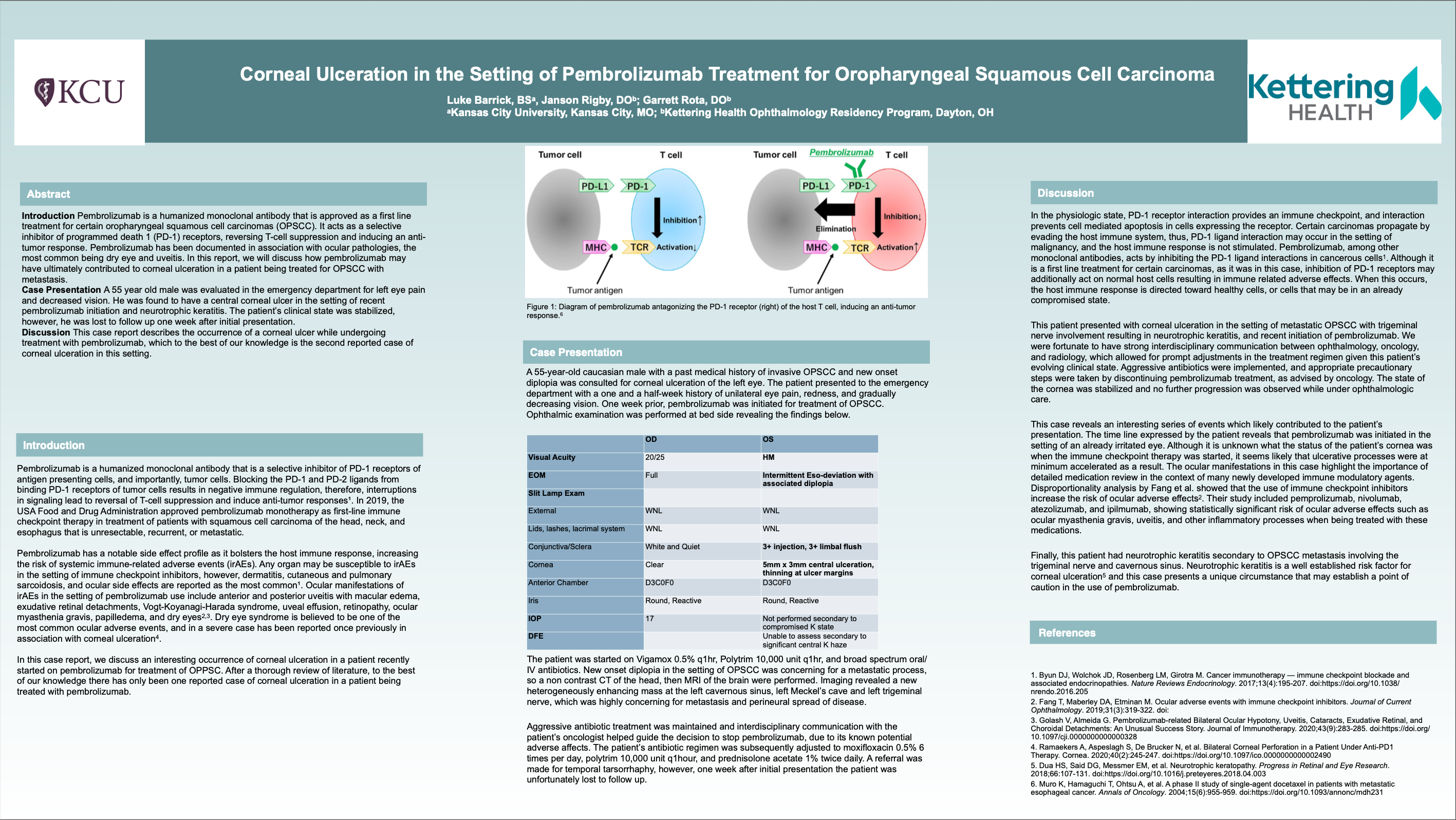
Pembrolizumab is a humanized monoclonal antibody that has been approved for first-line immune checkpoint therapy in treatment of patients with squamous cell carcinoma of the head, neck, and esophagus that is unresectable, recurrent, or metastatic. In this case report, we discuss an interesting occurrence of corneal ulceration in a patient recently started on pembrolizumab for the treatment of oropharyngeal squamous cell carcinoma. This case highlights the importance of caution when initiating treatment with immune checkpoint inhibitors, as well as the value of strong interdisciplinary communication, as seen in this case with ophthalmology, oncology, and radiology coordinating care for this patient.

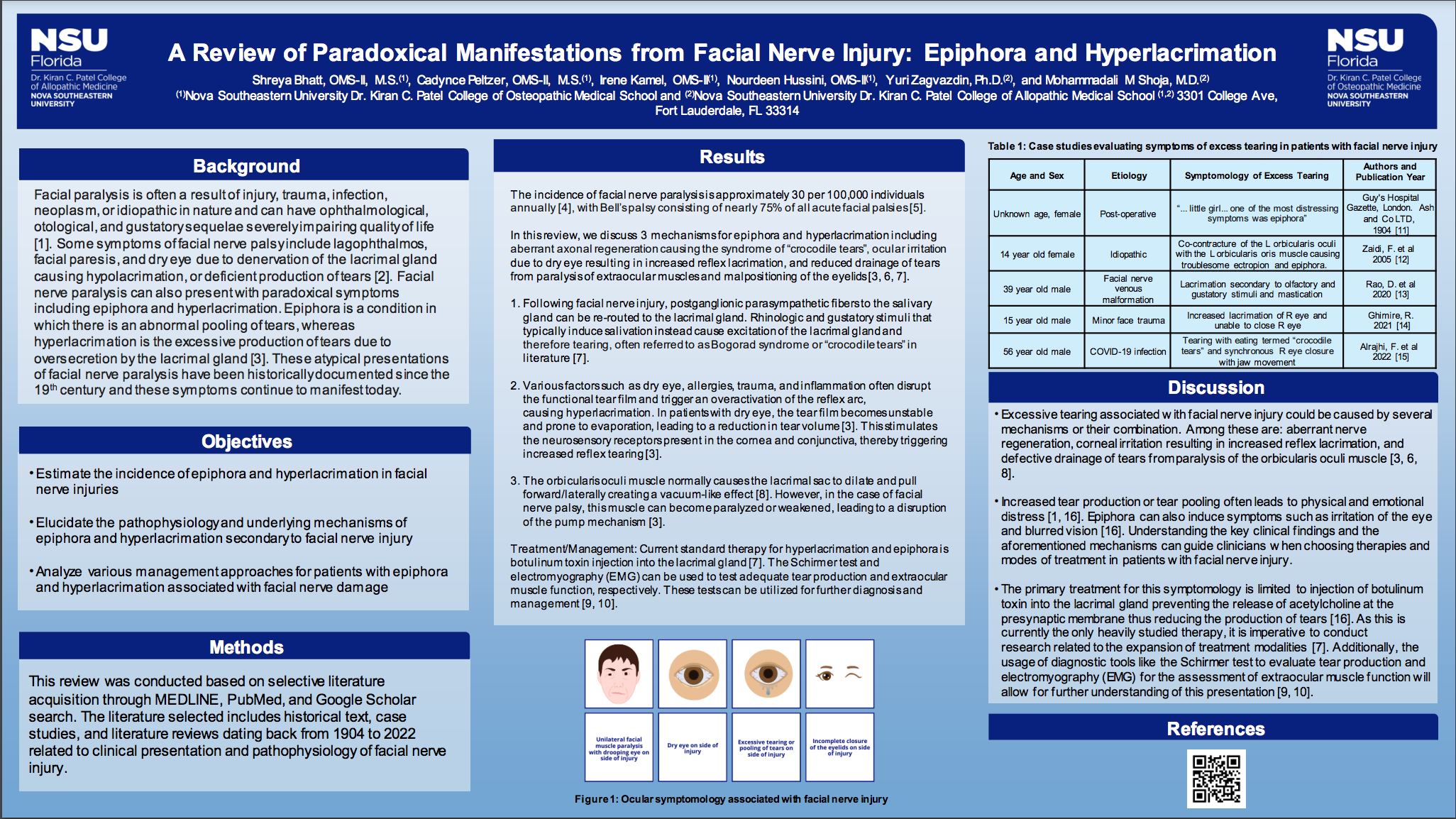
Shreya Bhatt MS
A Review of the Paradoxical Manifestations from Facial Nerve Injury: Epiphora and Hyperlacrimation
Shreya Bhatt is currently a second year medical student at Nova Southeastern University (NSU) Dr. Kiran C. Patel College of Osteopathic Medicine. She graduated with a Bachelor of Science degree in Neurobiology from Penn State University and received her Masters in Biomedical Sciences from NSU in 2021. She is very interested in pursuing ophthalmology after medical school and thoroughly enjoys conducting research in this field as well as Neurobiology and research related to the head and neck. Outside of her courses and research, Shreya is the president of her medical school’s Ophthalmology Club, Random Acts of Kindness organization, and the Medical Students for Individuals with Possibilities organization. She also serves as a peer mentor for the underclassmen, served as a Teaching Assistant in Public Health for the undergraduate students, and enjoys volunteering at various service events, baking, cooking, and spending time with friends and family in her spare time.
Abstract
View Abstract
Summary
The incidence of facial nerve paralysis is roughly 30 per 100,000 persons annually. Despite being frequently idiopathic in nature, as is commonly seen with Bell’s palsy, it may also be caused by infection, trauma, or neoplasm. It manifests with lagophthalmos, partial or total facial paresis, and dry eye due to denervation of the lacrimal gland alongside other ocular abnormalities. In this study, we examine the incidence and mechanisms of epiphora and hyperlacrimation in facial nerve injury by reviewing historical publications dating back to the 19th century as well as recent literature. Several mechanisms have been proposed, including aberrant axonal regeneration known to cause the syndrome of “crocodile tears”, ocular irritation due to dry eye with disruption of the tear film resulting in increased reflex lacrimation, and reduced drainage of tears as a result of paralysis of the orbicularis oculi muscle and malpositioning of the eyelids. The mechanisms of excess tearing in some types of facial nerve lesions, for example in patients with certain brainstem tumors, remain unknown. Understanding the pathophysiology of epiphora and hyperlacrimation is crucial in guiding management of patients presenting with these aforementioned signs of facial nerve injury. Further experimental and clinical studies focusing on the quantification of tear production and precise localization of facial nerve damage via modalities such as the Schirmer test and electromyography will help improve our understanding of these paradoxical manifestations from facial nerve dysfunction.

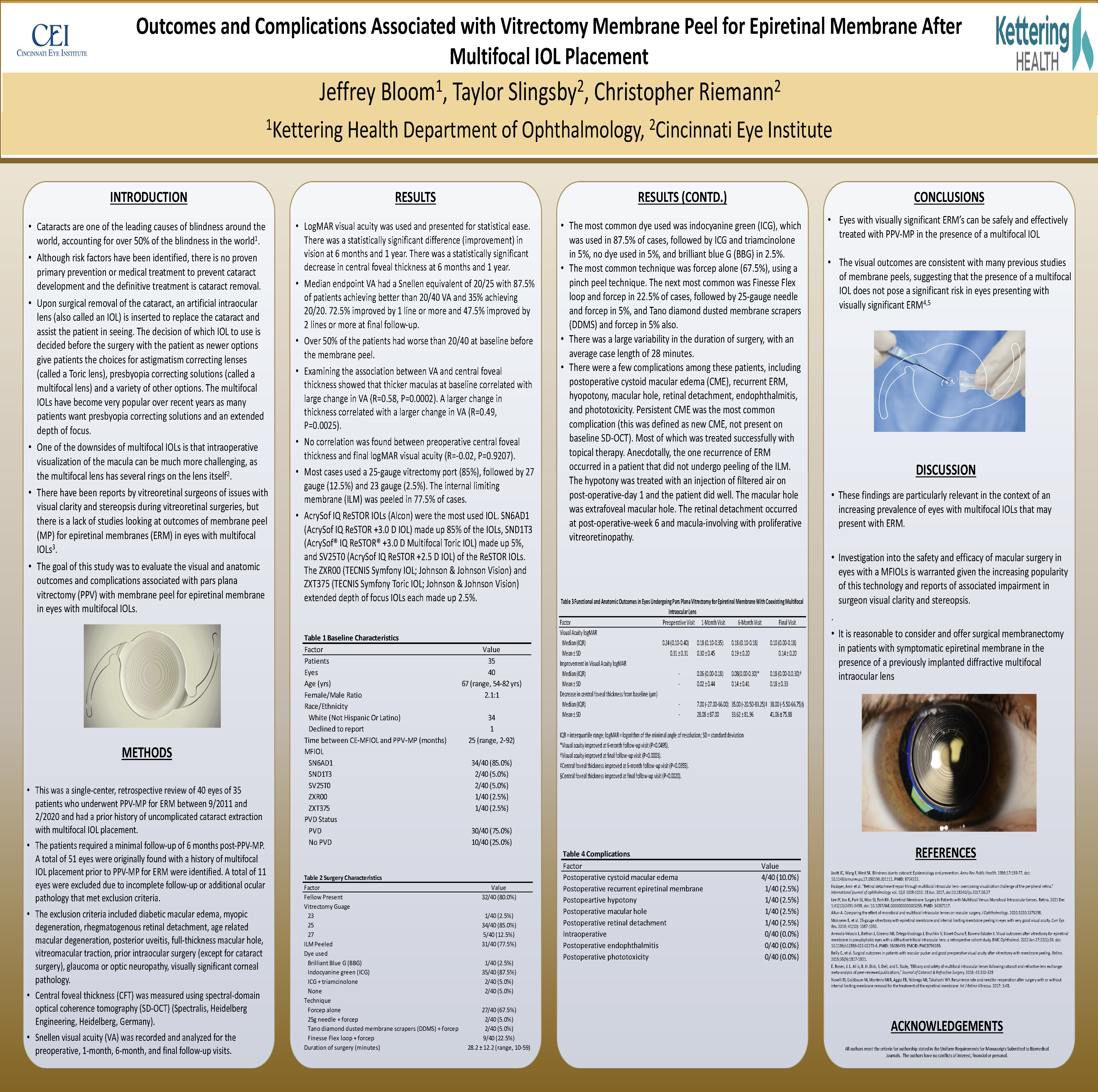
Jeffrey Bloom DO
Outcomes and Complications Associated with Vitrectomy Membrane Peel for Epiretinal Membrane After Multifocal IOL Placement
My name is Jeffrey Bloom, and I am a PGY-4 ophthalmology resident at Kettering Health- Dayton. In my free time I enjoy working out, hanging with friends, and perfecting my amateur barista skills. My plan for the future is a surgical retina fellowship at Acuity Eye Group in Pasadena, California!
Abstract
View Abstract
Summary
Cataracts are one of the leading causes of blindness around the world, accounting for over 50% of the blindness in the world. Although risk factors have been identified, there is no proven primary prevention or medical treatment to prevent cataract development and the definitive treatment is cataract removal. Upon surgical removal of the cataract, an artificial intraocular lens (also called an IOL) is inserted to replace the cataract and assist the patient in seeing. The decision of which IOL to use is decided before the surgery with the patient as newer options give patients the choices for astigmatism correcting lenses (called a Toric lens), presbyopia correcting solutions (called a multifocal lens) and a variety of other options. One of the downsides of multifocal IOLs is that intraoperative visualization of the macula can be much more challenging, as the multifocal lens has several rings on the lens itself. There have been reports by vitreoretinal surgeons of issues with visual clarity and stereopsis during vitreoretinal surgeries, but there is a lack of studies looking at outcomes of membrane peel (MP) for epiretinal membranes (ERM) in eyes with multifocal IOLs. The goal of this study was to evaluate the visual and anatomic outcomes and complications associated with pars plana vitrectomy (PPV) with membrane peel for epiretinal membrane in eyes with multifocal IOLs. The study demonstrated that eyes with visually significant ERM’s can be safely and effectively treated with PPV-MP in the presence of a multifocal IOL. The visual outcomes of the study are consistent with many previous studies of membrane peels, suggesting that the presence of a multifocal IOL does not pose a significant risk in eyes presenting with visually significant ERM.

Jacqueline Erdahl DO
Pembrolizumab Induced Myasthenia Gravis; A case report
I am originally from middle of the mitten, Mount Pleasant, MI, and completed bachelors degree in Physiology at Michigan State University. After completing medical school at ATSU-KCOM, where I met my husband Luke who is know an Emergency Medicine Physician, we have made a home with the fluffiest golden retriever and cutest one year old son in Dayton, OH. Upon anticipated to graduation from residency at Kettering Health Dayton this summer, I plan to stay in the area to assist training future residents and give back to the amazing program that trained me.
Abstract
View Abstract
Summary
Luckily, life threatening conditions are not frequently presenting to the eye clinic, but early identification and treatment is of utmost importance when they do. One of these rare, but on the rise conditions, is immune check point inhibitor(ICI) related adverse events. Here we present a fatal case report of Pembrolizumab induced Myasthenia Gravis. Pembrolizumab is an ICI used to decrease mortality in cancer patients, but with a risk of rare potentially fatal immune-related adverse events that are still under investigation. The treatment of variety of malignancies now can involve ICIs and recent studies on potential monitoring for immune related adverse events with neuromuscular antibody testing have been published.

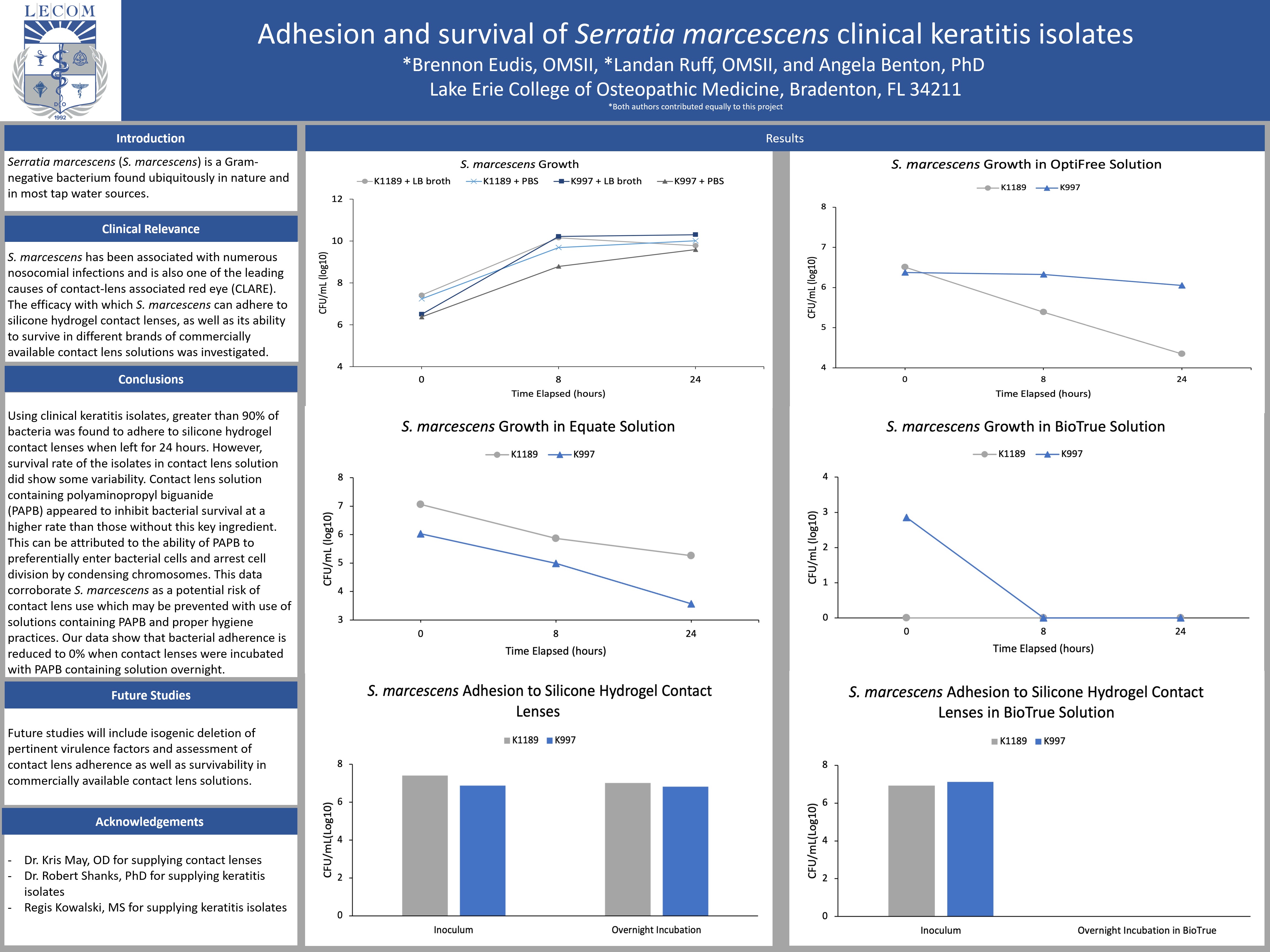
Brennon Eudis M.M.S.
Adhesion and survival of Serratia marcescens clinical keratitis isolates
OMSII at Lake Erie College of Osteopathic Medicine Bradenton
Abstract
View Abstract
Summary
Adhesion and survival of Serratia marcescens was investigated in several different contact lens solutions.

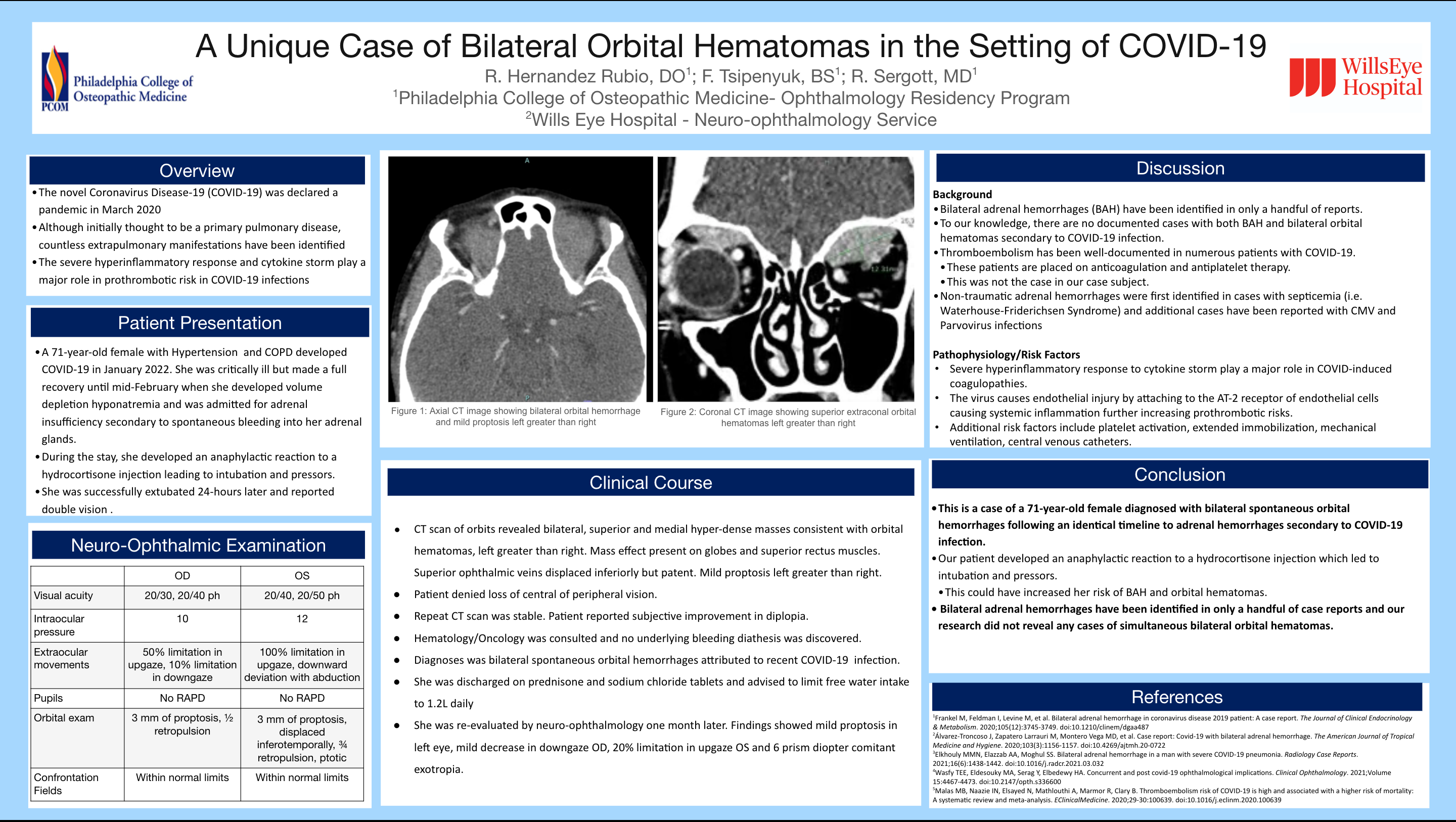
Raul Hernandez Rubio DO
A Unique Case of Bilateral Orbital Hematomas in the Setting of COVID-19: A Case Report
3rd time presenting at AOCOO-HNS and excited to present this unique case.
I was raised in Puerto Rico and decided to pursue ophthalmology after realizing my passion for both art and surgery. I am currently the chief ophthalmology resident at PCOM and will be doing an oculoplastic surgery fellowship at Kaiser Permanente under Dr. Kimberly Cockerham.
Education:
Cornell University BS
GA-PCOM DO
PCOM Ophthalmology Residency
Hobbies:
Purebred dog handler (proud dad of Penelope and Valerie)
Wildlife Photography
Avid Boston Celtics Fan
Abstract
View Abstract
Summary
The novel Coronavirus Disease-19 (COVID-19) was declared a pandemic in March 2020. Although initially thought to be a primary pulmonary disease, countless extrapulmonary manifestations have been identified. In this Case Report we discuss a 71 year old female presenting with bilateral orbital hematomas and adrenal hemorrhages shortly after recovering from COVID-19 infection.

Cameron Holicki DO
A Unique Case of Bilateral Endogenous Endophthalmitis
Abstract
View Abstract
Summary
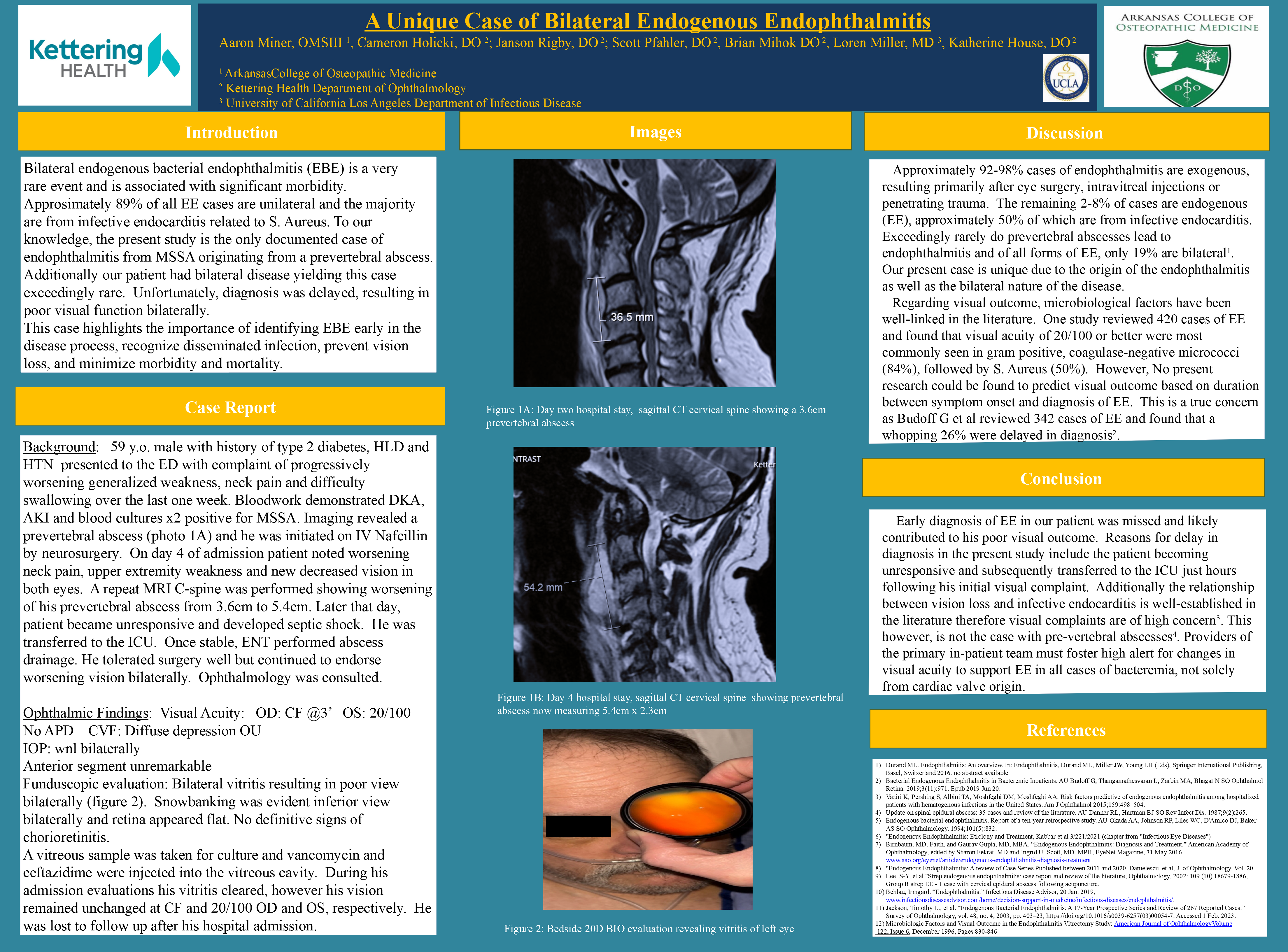
Bilateral endogenous bacterial endophthalmitis (EBE) is a very
rare event and is associated with significant morbidity. Approsimately 89% of all EE cases are unilateral and the majority are from infective endocarditis related to S. Aureus. To our knowledge, the present study is the only documented case of endophthalmitis from MSSA originating from a prevertebral abscess. Additionally our patient had bilateral disease yielding this case exceedingly rare. Unfortunately, diagnosis was delayed, resulting in poor visual function bilaterally.
This case highlights the importance of identifying EBE early in the disease process, recognize disseminated infection, prevent vision loss, and minimize morbidity and mortality.
Katelyn Joubert DO
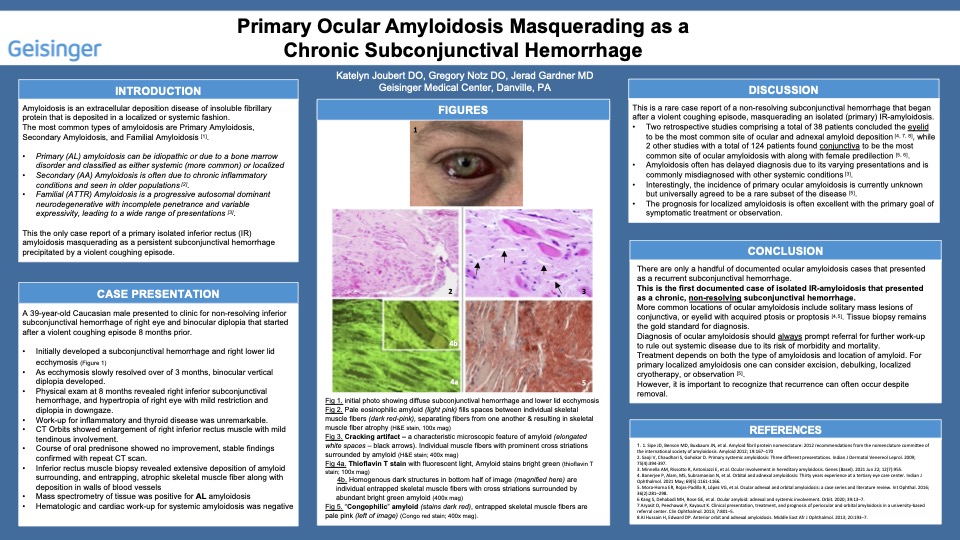
Primary Ocular Amyloidosis Masquerading as a Chronic Subconjunctival Hemorrhage
Summary

Caleb Liles D.O.
A Rare Case of Occipital Lobe Involvement in Onchocerciasis
PGY-2 at Kettering Health Ophthalmology
Abstract
View Abstract
Summary
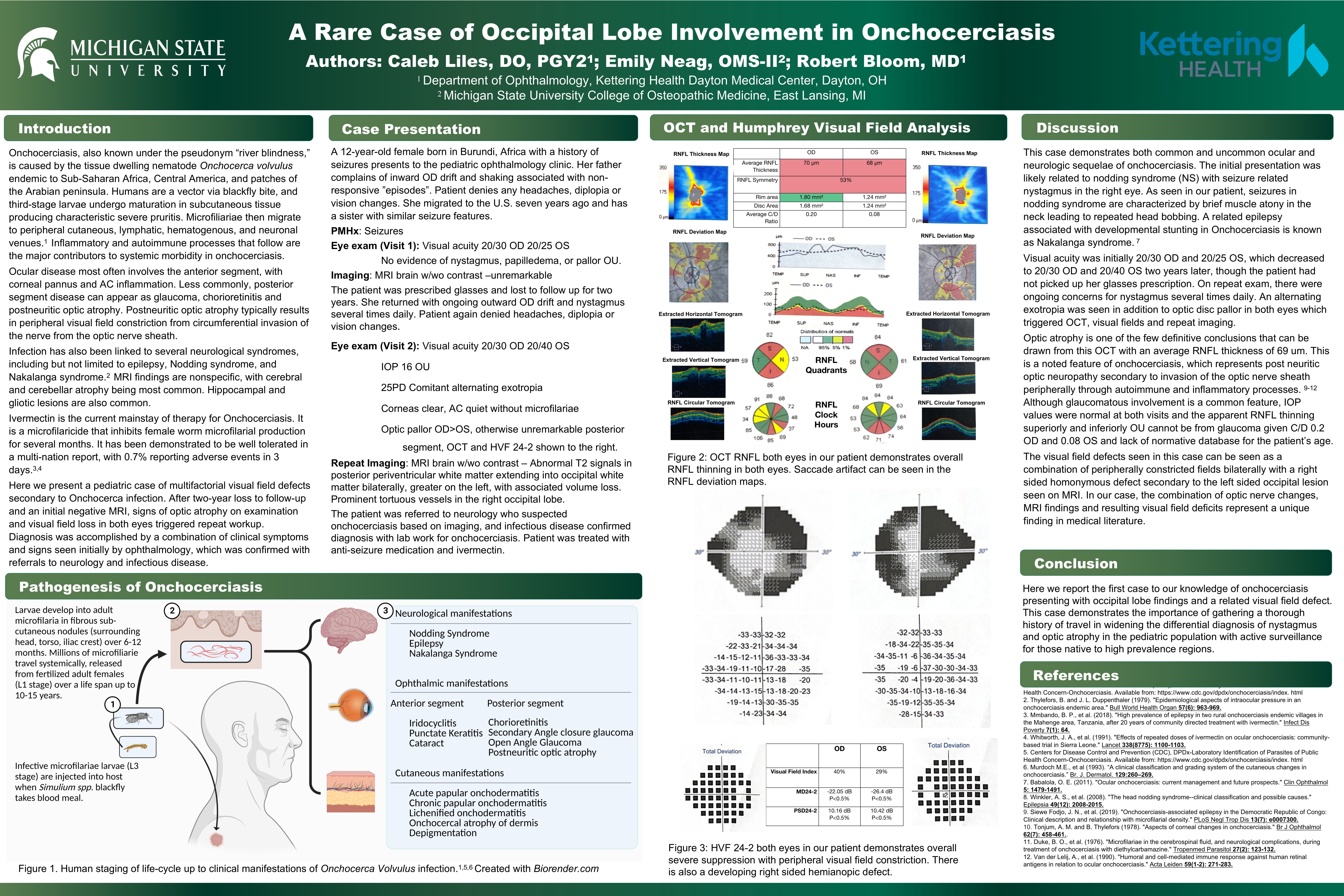
Onchocerciasis, also known as “river blindness”, is caused by the nematode Onchocerca volvulus endemic to Sub-Saharan Africa, Central America, and parts of the Arabian Peninsula. Microfilariae are introduced to the skin via the blackfly bite, which then migrate through various avenues to create cutaneous, neurologic and ophthalmic complications.
The ophthalmologist can be the first provider to recognize sequelae of this disease and should direct the appropriate workup including MRI of the brain and referrals to neurology and infectious disease if suspicion remains high. In our patient this was the case. This 12 year old female patient from Africa presented with concerns for intermittent nystagmus of the right eye associated with “staring spells”. Unfortunately, after the patient was initially seen and the MRI was unremarkable, the patient was lost to follow up for two years. She then presented with later sequelae involving postneuritic optic neuropathy and a rare finding of occipital lobe involvement and related visual field defects that might have been improved with earlier treatment with ivermectin.
Here we report the first case to our knowledge of occipital lobe involvement in onchocerciasis causing a homonymous visual field defect. This case demonstrates the importance of gathering a thorough travel history in evaluating a pediatric patient with findings of nystagmus and optic atrophy.
Brian Nguyen DO
Idiopathic Unilateral Choroidal Neovascularization in a Young Female
Abstract
View Abstract
Summary
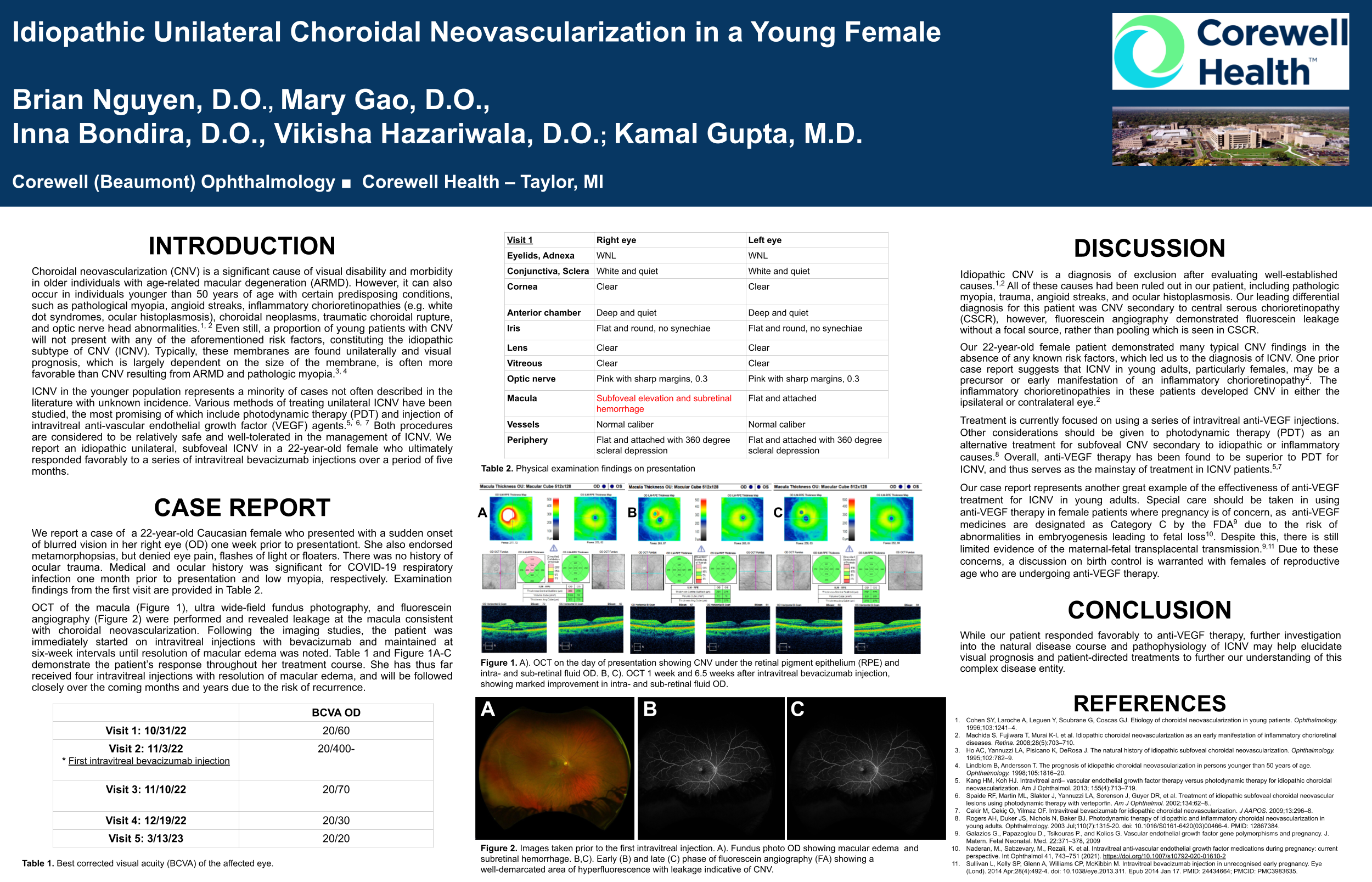
Choroidal neovascularization (CNV) is a significant cause of visual disability and morbidity in older individuals with age-related macular degeneration (ARMD). However, it can also occur in individuals younger than 50 years of age with certain predisposing conditions, such as pathological myopia, angioid streaks, inflammatory chorioretinopathies (e.g. white dot syndromes, ocular histoplasmosis), choroidal neoplasms, traumatic choroidal rupture, and optic nerve head abnormalities. Even still, a proportion of young patients with CNV will not present with any of the aforementioned risk factors, constituting the idiopathic subtype of CNV (ICNV). Typically, these membranes are found unilaterally and visual prognosis, which is largely dependent on the size of the membrane, is often more favorable than CNV resulting from ARMD and pathologic myopia.
ICNV in the younger population represents a minority of cases not often described in the literature with unknown incidence. Various methods of treating unilateral ICNV have been studied, the most promising of which include photodynamic therapy (PDT) and injection of intravitreal anti-vascular endothelial growth factor (VEGF) agents. Both procedures are considered to be relatively safe and well-tolerated in the management of ICNV. We report an idiopathic unilateral, subfoveal ICNV in a 22-year-old female who ultimately responded favorably to a series of intravitreal bevacizumab injections over a period of five months.

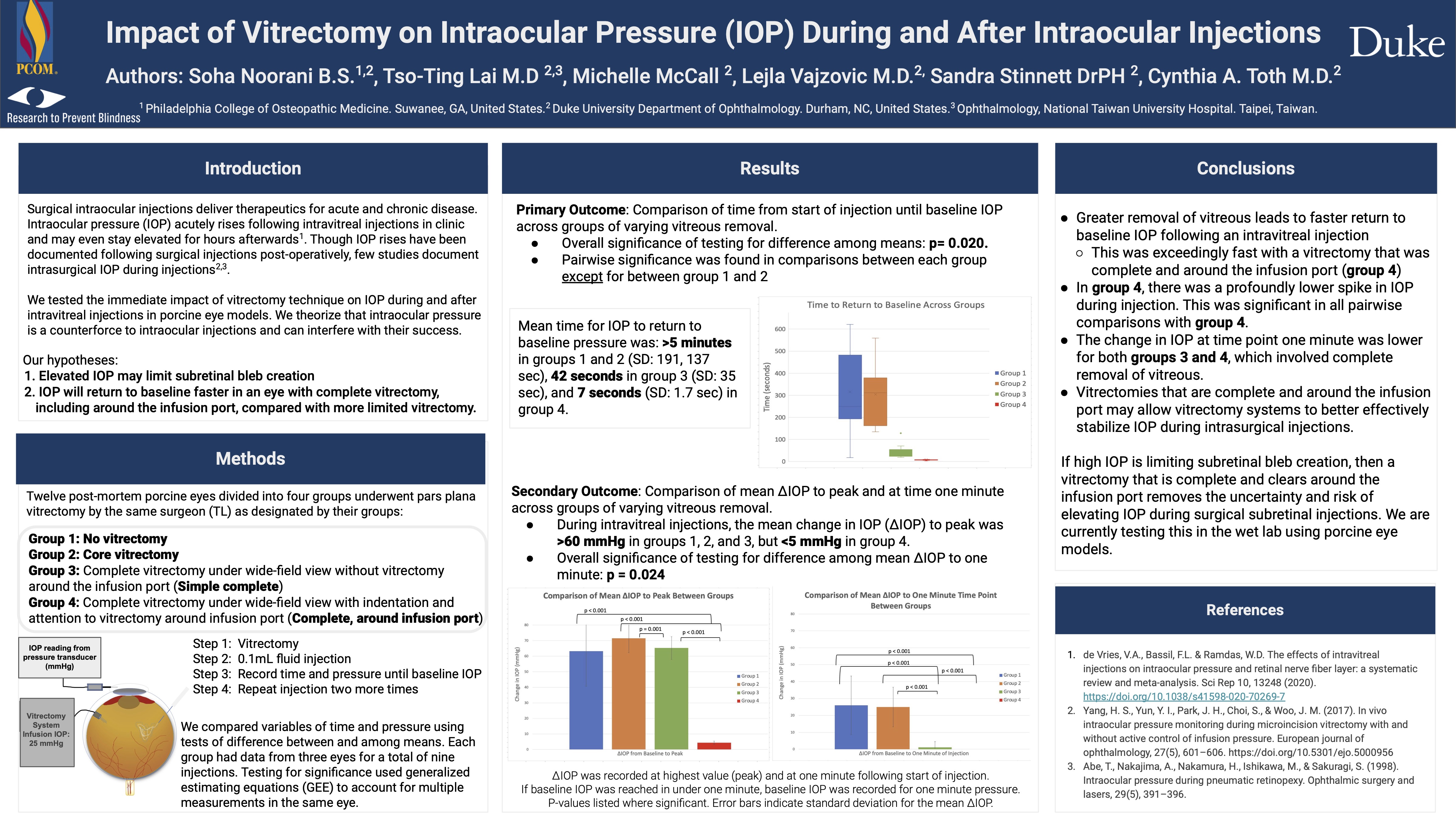
Soha Noorani OSM4
Impact of Vitrectomy on Intraocular Pressure (IOP) During and After Intraocular Injections
Abstract
View Abstract
Summary
This study looked at the impact of vitreous removal on subsequent intraocular pressure (IOP) changes during intra-surgical injections into the vitreous cavity. We hypothesized that thorough vitreous removal, with specific attention to vitrectomy around the infusion port, would yield a faster stabilization of IOP as controlled by the infusion source on the vitrectomy machine. In order to study this, we divided porcine eyes into groups based on extent of vitreous removal, and then administered a fluid injection of set amount while recording IOP from a pressure transducer connected to the anterior chamber.
While comparing these groups of varying vitrectomies, we found that the group that had had complete vitreous removal with vitrectomy around the infusion port exhibited lower spikes of IOP during the injection compared to the other groups that had undergone less extensive vitrectomy. We also saw that the pressure returned to baseline faster in this group compared to the others. This study showed that a complete vitrectomy with specific attention to the infusion port removes the risk of elevating IOP during injections. This information is particularly helpful in the setting of subretinal injections, as factors such as IOP may impact successful bleb formation.

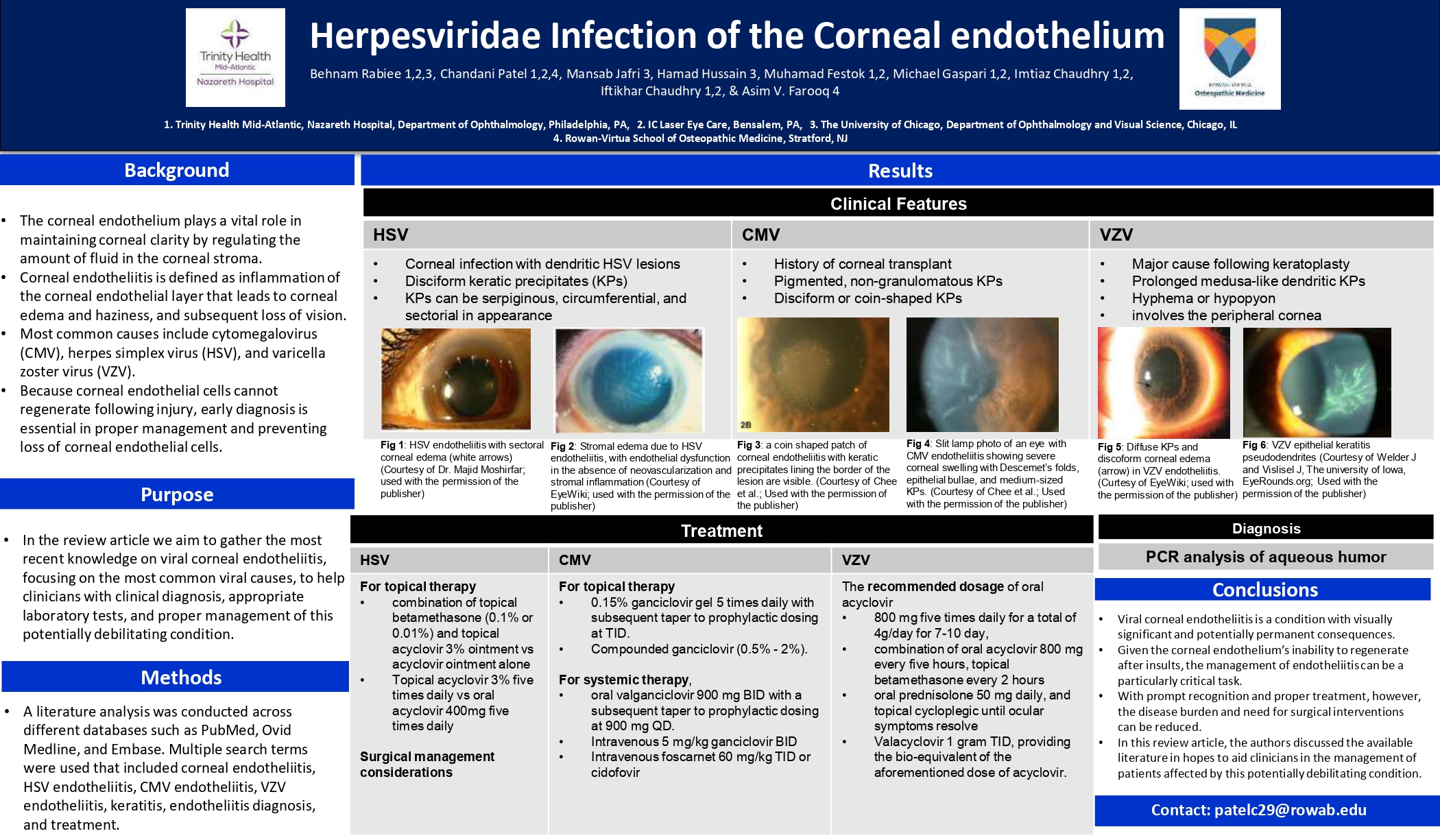
Chandani Patel DO
Herpesviridae infections of the corneal endothelium
I was born and raised in India and moved to the United States in 2013. I attended New Jersey Institute of Technology on a scholarship with Albert Dorman Honors College. I graduated with cum laude and I'm currently a third year medical student at Rowan-Virtua School of Osteopathic Medicine. Outside of school, I enjoy working out, pilates, playing tennis, cooking, reading, writing, and art.
Abstract
View Abstract
Summary
Corneal endotheliitis is an inflammatory process, most commonly of viral etiology, that manifests clinically with features, including corneal edema, keratic precipitates, and a mild anterior chamber reaction. The pathogenesis of endotheliitis has yet to be fully elucidated. Several studies have implicated human herpesviruses from the Herpesviridae family as primary causes of corneal endotheliitis, including, herpes simplex viruses 1 and 2 (HSV-1 and HSV-2), cytomegalovirus (CMV), and varicella zoster virus (VZV). This review critically evaluates the present literature surrounding Herpesviridae infections of the corneal endothelium, including clinical manifestations, laboratory techniques, and treatment modalities.

Cadynce Peltzer M.S., OMS-II
The Association between Congenital Cataract Incidence and Average Ambient Temperature in Florida by County from 2008 to 2018
Cadynce Peltzer is a second-year osteopathic medical student at Nova Southeastern University Kiran C. Patel College of Osteopathic Medicine and has experience in clinical trials, retina, and optometric technician tasks. She holds a Bachelor of Science degree in Microbiology and Cell Science from the University of Florida and a Master of Science degree in Medical Science from the University of South Florida. Peltzer is also a second lieutenant in the United States Air Force and serves as a member of executive board for her military club(SAMOPS) chapter.
She is involved in the honors anatomy fellowship at her medical school where she teaches gross anatomy to first year students in laboratories by using digital technology and applications. In addition to this commitment, she has donated over 200 hours to service and volunteer missions over the last two years to help other military families, the aging population, and people in mental health crisis within her community.
During the weekend, she like to spend time outdoors with her dogs Hudson and Honey or bake sourdough bread for her friends and neighbors.
Abstract
View Abstract
Summary
Maternal heat exposure and high environmental temperatures during gestational periods have been known to cause an assortment of congenital complications. Some of these health-related adversities include hypospadias, spina bifida, cleft palate, and congenital cataracts, also known as infantile cataracts. While genetic mutation remains the most common etiology for congenital cataracts, other potential risk factors include metabolic disorder, prenatal infection, trauma, and environmental influence such as atmospheric torridity. In this analysis, we investigated the correlation between summer heat in Florida on expectant mothers and congenital cataract formation in newborns. Using a polynomial regression model and available congenital malformation data from the Florida Department of Health, we analyzed the relationship between infantile cataracts and average ambient degrees in Fahrenheit. Our model revealed a significant correlation between temperature and congenital cataracts. Because congenital cataracts are one of the leading causes of visual loss in children worldwide, it is paramount to educate pregnant patients on risks and precautions in order to reduce blindness among infants.

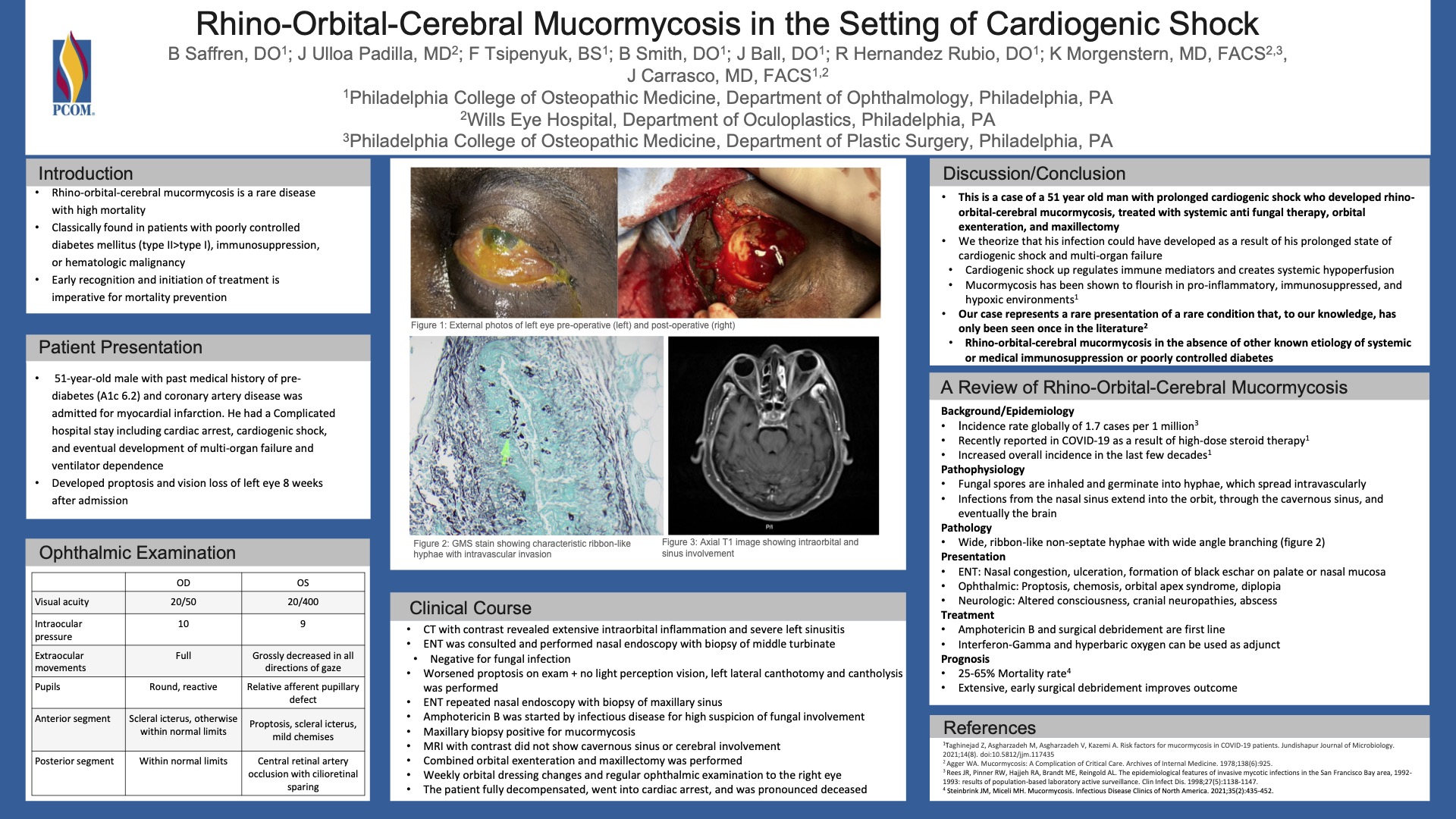
Brooke Saffren DO
Rhino-Orbital-Cerebral Mucormycosis in the Setting of Cardiogenic Shock
I am a current PGY-2 resident in ophthalmology at Philadelphia College of Osteopathic Medicine. Prior to residency, I went to medical school at Philadelphia College of Osteopathic Medicine and did a year-long research fellowship at Wills Eye Hospital in the department of Pediatric Ophthalmology and Ocular Genetics. For undergraduate education, I attended Rochester Institute of Technology with a major in biomedical science and a minor in imaging science.
Abstract
View Abstract
Summary
Rhino-orbital-cerebral mucormycosis is a rare disease caused by fungal angioinvasion of the orbit, cavernous sinus, and eventually the brain. It commonly presents in patients with poorly controlled diabetes or who are immunocompromised. We present a patient who developed rhino-orbital-cerebral mucormycosis in the setting of prolonged cardiogenic shock. This, to our knowledge, has only been reported once in the literature and represents a rare presentation of an already rare disease. We also present a literature review of epidemiology, pathophysiology, histopathology and current management recommendations for mucormycosis.

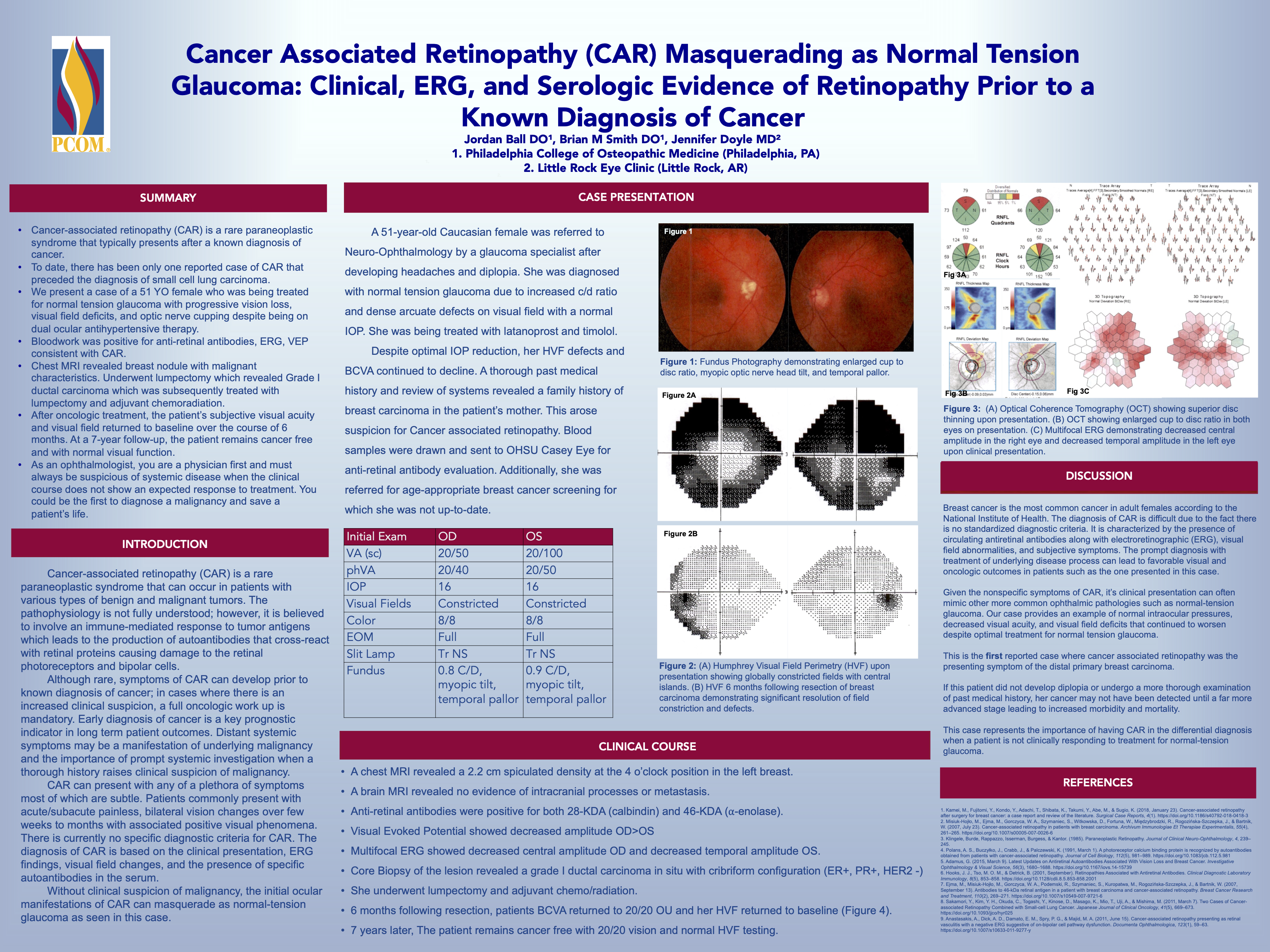
Brian Smith DO
Cancer Associated Retinopathy (CAR) Masquerading as Normal Tension Glaucoma: Clinical, ERG, and Serologic Evidence of Retinopathy Prior to a Known Diagnosis of Cancer
PGY-3
Abstract
View Abstract
Summary
Cancer-associated retinopathy (CAR) is a rare paraneoplastic syndrome that typically presents after a known diagnosis of cancer.
To date, there has been only one reported case of CAR that preceded the diagnosis of small cell lung carcinoma. We present a case of a 51 YO female who was being treated for normal tension glaucoma with progressive vision loss, visual field deficits, and optic nerve cupping despite being on dual ocular antihypertensive therapy. Bloodwork was positive for anti-retinal antibodies, ERG, VEP consistent with CAR. Chest MRI revealed breast nodule with malignant characteristics. Underwent lumpectomy which revealed Grade I ductal carcinoma which was subsequently treated with lumpectomy and adjuvant chemoradiation. After oncologic treatment, the patient’s subjective visual acuity and visual field returned to baseline over the course of 6 months. At a 7-year follow-up, the patient remains cancer free and with normal visual function. As an ophthalmologist, you are a physician first and must always be suspicious of systemic disease when the clinical course does not show an expected response to treatment. You could be the first to diagnose a malignancy and save a patient’s life.

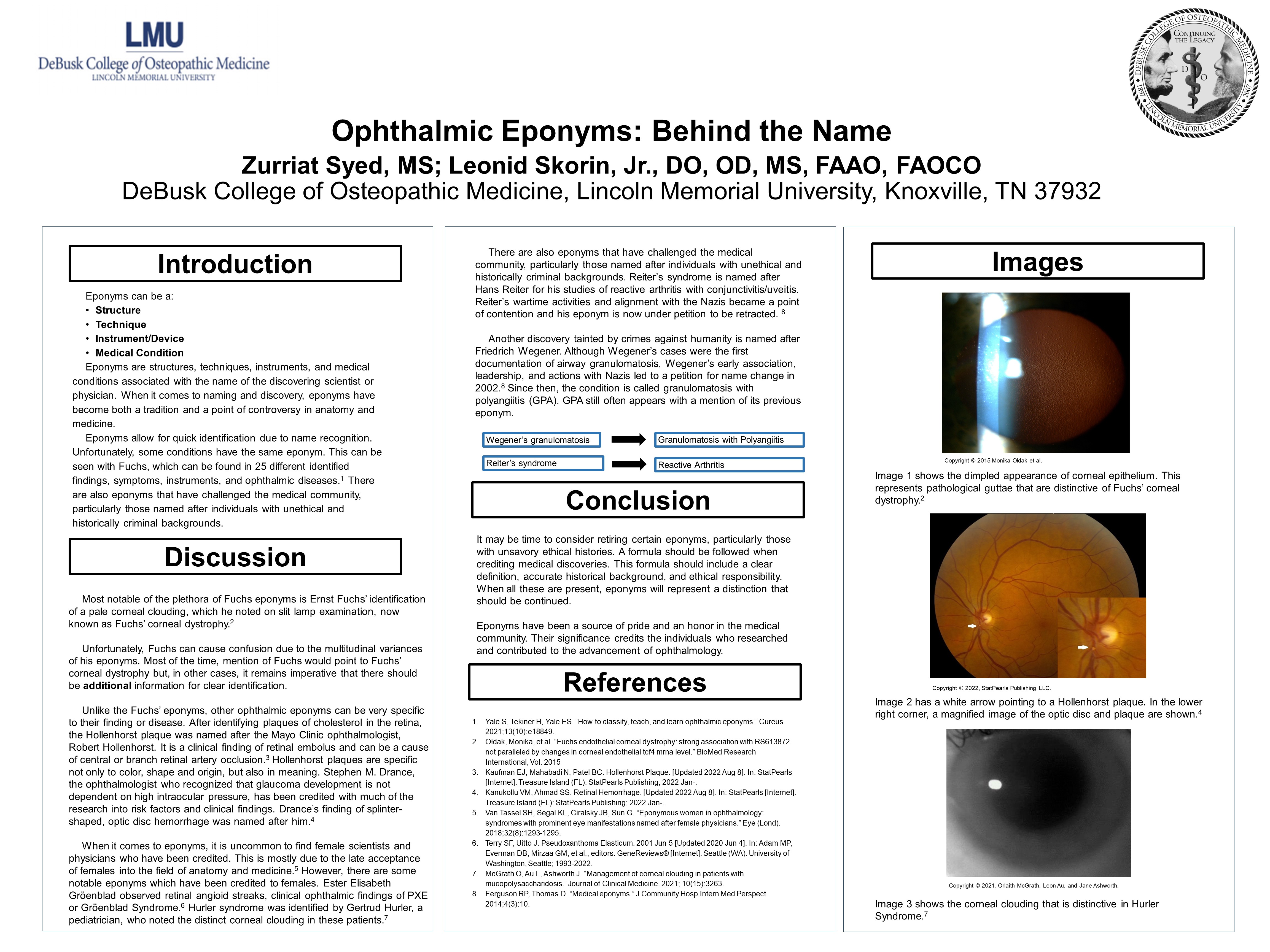
Zurriat Syed M.S.
Ophthalmic Eponyms: Behind the Name
Zurriat Syed is a medical student at Lincoln Memorial University DeBusk College of Osteopathic Medicine. She is a graduate of University of California, Berkeley with a bachelor’s degree in molecular cell biology and a master’s in science.
Abstract
View Abstract
Summary
Eponyms are structures, techniques, instruments, and medical conditions associated with the name of the discovering scientist or physician. When it comes to naming and discovery, eponyms have become both a tradition and a point of controversy in anatomy and medicine. Arguments against them have stemmed from named individuals’ unethical actions and backgrounds, evolving definitions, and inaccuracy with language differences. Eponyms abound in ophthalmology from instruments, pathologies to anatomical eye structures. It may be time to consider retiring certain eponyms, particularly those with unsavory ethical histories. A formula should be followed when crediting medical discoveries. This formula should include a clear definition, accurate historical background, and ethical responsibility. When all these are present, eponyms will represent a distinction that should be continued. Eponyms have been a source of pride and an honor in the medical community. Their significance credits the individuals who researched and contributed to the advancement of ophthalmology.
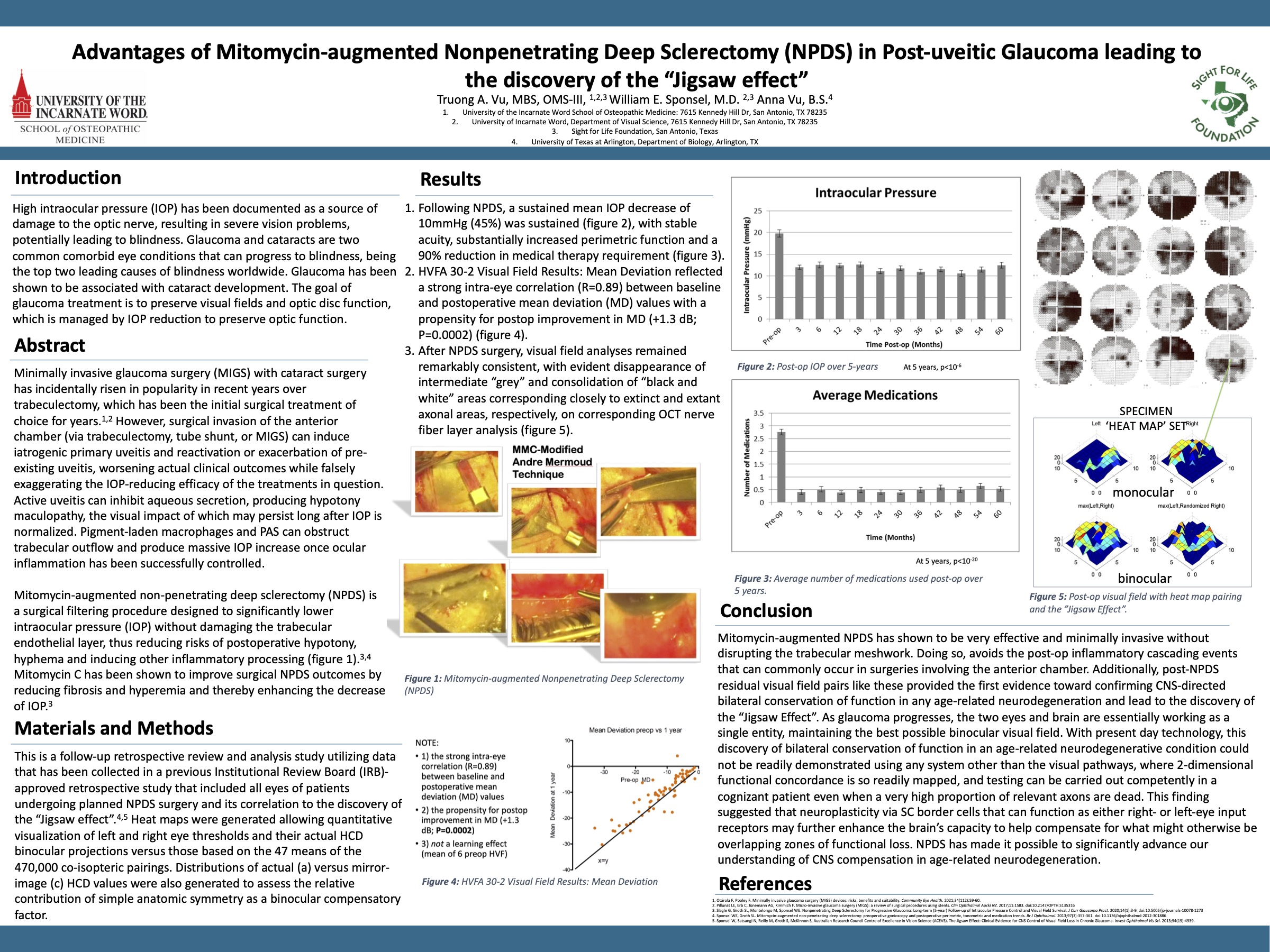
Truong A. Vu MBS, OMS3
Advantages of Mitomycin-augmented Nonpenetrating Deep Sclerectomy (NPDS) in Post-uveitic Glaucoma leading to the discovery of the “Jigsaw effect”
Abstract
View Abstract
Summary
High intraocular pressure (IOP) has been documented as a source of damage to the optic nerve, resulting in severe vision problems, potentially leading to blindness. Glaucoma and cataracts are two common comorbid eye conditions that can progress to blindness, being the top two leading causes of blindness worldwide. Glaucoma has been shown to be associated with cataract development. The goal of glaucoma treatment is to preserve visual fields and optic disc function, which is managed by IOP reduction to preserve optic function. Mitomycin-augmented non-penetrating deep sclerectomy (NPDS) is a surgical filtering procedure designed to significantly lower intraocular pressure (IOP) without damaging the trabecular endothelial layer, thus reducing risks of postoperative hypotony, hyphema and inducing other inflammatory processing. Mitomycin C has been shown to improve surgical NPDS outcomes by reducing fibrosis and hyperemia and thereby enhancing the decrease of IOP. Post-NPDS residual visual field pairs like these provided the first evidence toward confirming CNS-directed bilateral conservation of function in any age-related neurodegeneration and lead to the discovery of the “Jigsaw Effect”.

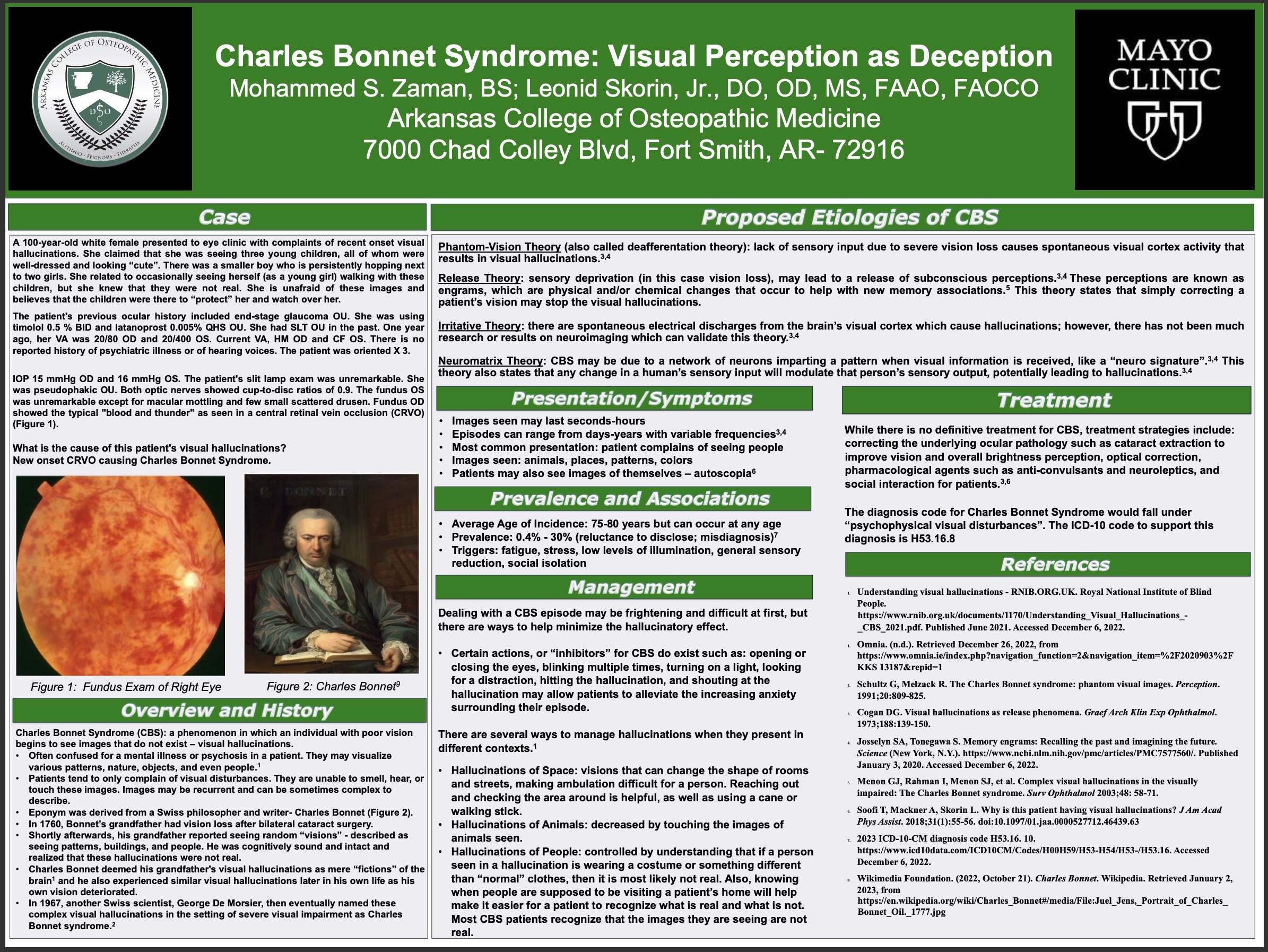
Mohammed Zaman BS
Charles Bonnet Syndrome: Visual Perception as Deception
Mohammed Zaman is currently a medical student at the Arkansas College of Osteopathic Medicine. He is a graduate of Illinois State University with a Bachelor's degree in Exercise Science.
Abstract
View Abstract
Summary
Charles Bonnet syndrome (CBS) is a phenomenon in which an individual with poor vision begins to see images that do not exist – visual hallucinations. These visual hallucinations can often be confused for a mental illness or psychosis in a patient. They may visualize various patterns, nature, objects, and even people. Patients who experience CBS tend to only complain of visual disturbances. They are unable to smell, hear, or touch these images. However, these images may be recurrent and can be sometimes complex to describe. Patients with CBS recognize that the images they are seeing are not real even though they are very vivid. CBS only affects sight, so they can be reassured if there are no delusions or other senses such as smell, or sound present associated with the hallucination. This presentation provides an investigation into CBS and its various etiologies, presenting symptoms, and methods of management for patients.

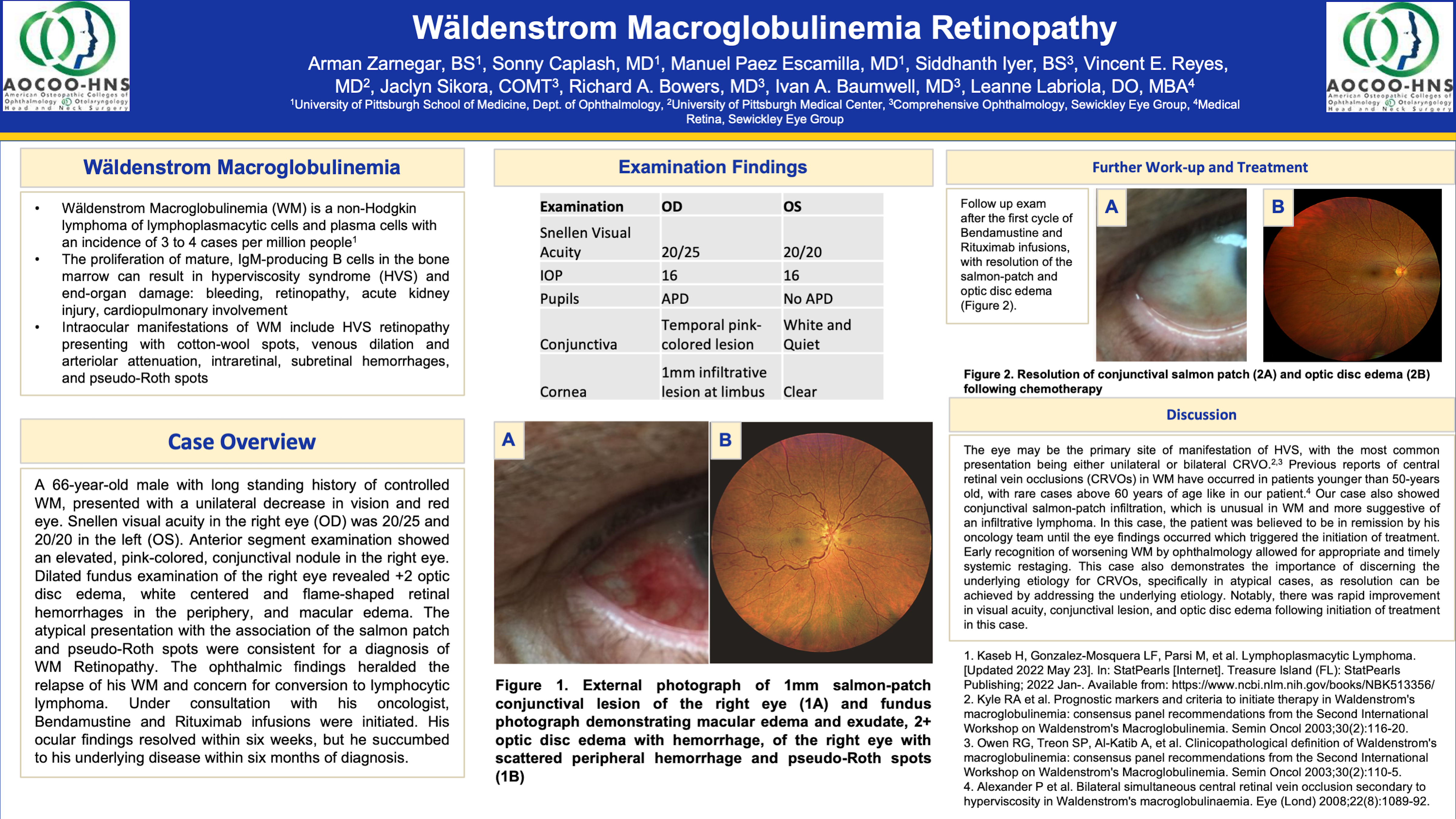
Arman Zarnegar BS
Wäldenstrom Macroglobulinemia Retinopathy
Arman is a current second-year medical student at the University of Pittsburgh School of Medicine. He is passionate about clinical service, mentorship, and ophthalmic research.
Abstract
View Abstract
Summary
Wäldenstrom Macroglobulinemia (WM) is a non-Hodgkin lymphoma characterized by the proliferation of IgM-producing B cells which can cause hyperviscosity syndrome (HVS) and, ultimately, end-organ damage. Herein, we describe a case of a patient with a history of long-standing WM who presented with signs of atypical central retinal vein occlusion (CRVO) and a salmon-patch conjunctival lesion that heralded relapse of his WM and concern for conversion to lymphocytic lymphoma. Upon consultation with his oncologist, a course of Bendamustine and Rituximab infusions was initiated, resulting in the resolution of his ocular findings in six weeks. Early recognition of worsening WM by ophthalmology allowed for appropriate and timely systemic restaging. Notably, there was rapid improvement in visual acuity, conjunctival lesion, and optic disc edema following the initiation of treatment in this case.

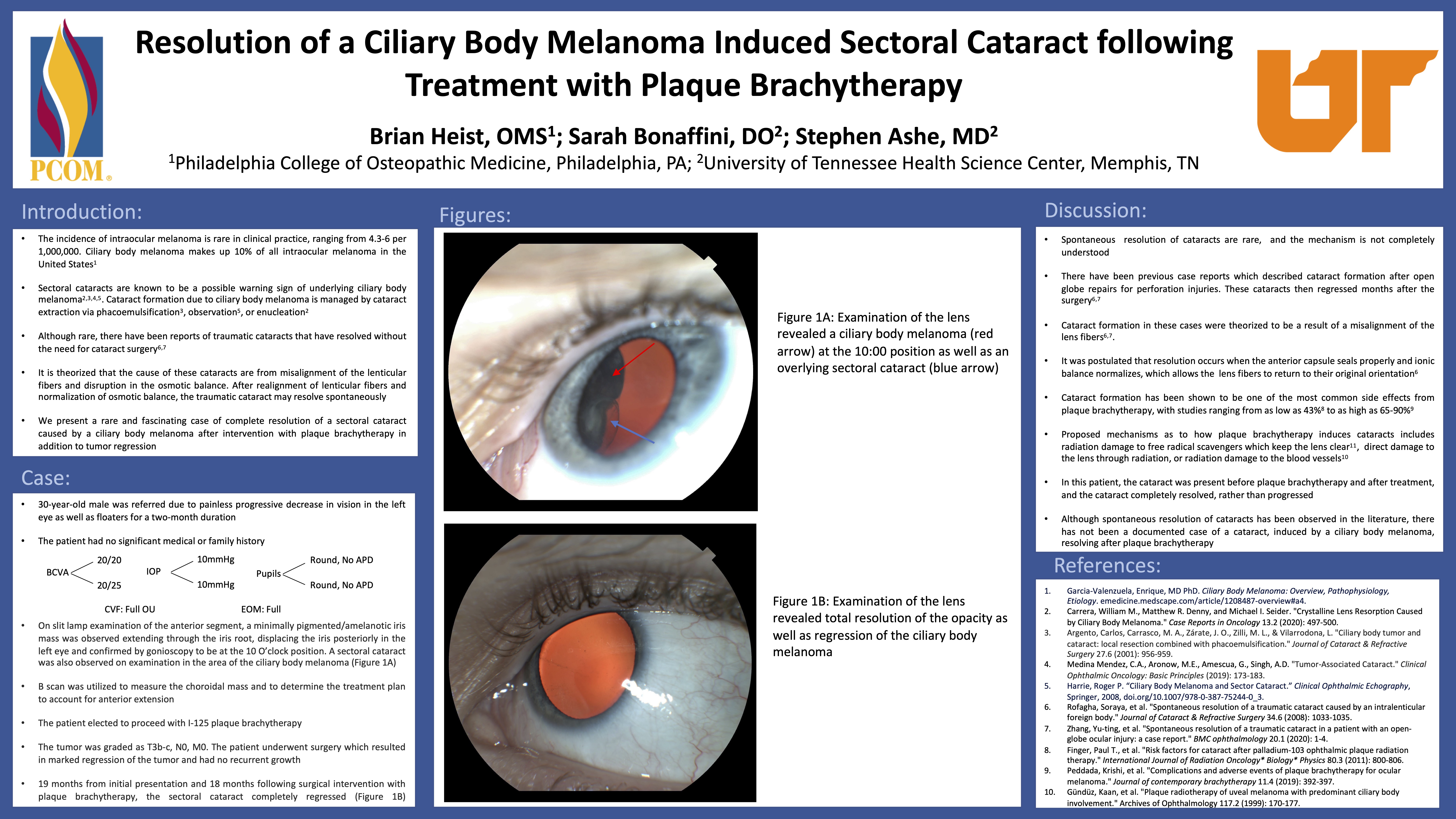
brian heist OMS
Resolution of a Ciliary Body Melanoma Induced Sectoral Cataract following Treatment with Plaque Brachytherapy
I am a 4th-year medical student at Philadelphia College of Osteopathic Medicine who is interested in pursuing a residency in ophthalmology. I am taking a gap year after medical school to do a year of ophthalmology research. I have previously volunteered at Wills Eye Surgical Center and currently working part-time as an ophthalmic tech, which I started doing in college.
Abstract
View Abstract
Summary
A 30-year-old male presented to an outside eye care provider for floaters and decreased visual acuity and was subsequently referred to ocular oncology service. His visual acuity was 20/20 on the right and 20/25 on the left. The patient was found to have a left ciliary body choroidal melanoma abutting the lens causing a sectoral cataract. After proceeding with iodine-125 plaque brachytherapy the tumor regressed and visual acuity improved. Less than a year later, the cataract spontaneously resolved. It is theorized that the cataract formed as a result of tumor apposition on the lens, causing a focal cataract. To our knowledge, this is the first case of a focal cataract caused by a ciliary body melanoma resulting in spontaneous resolution.

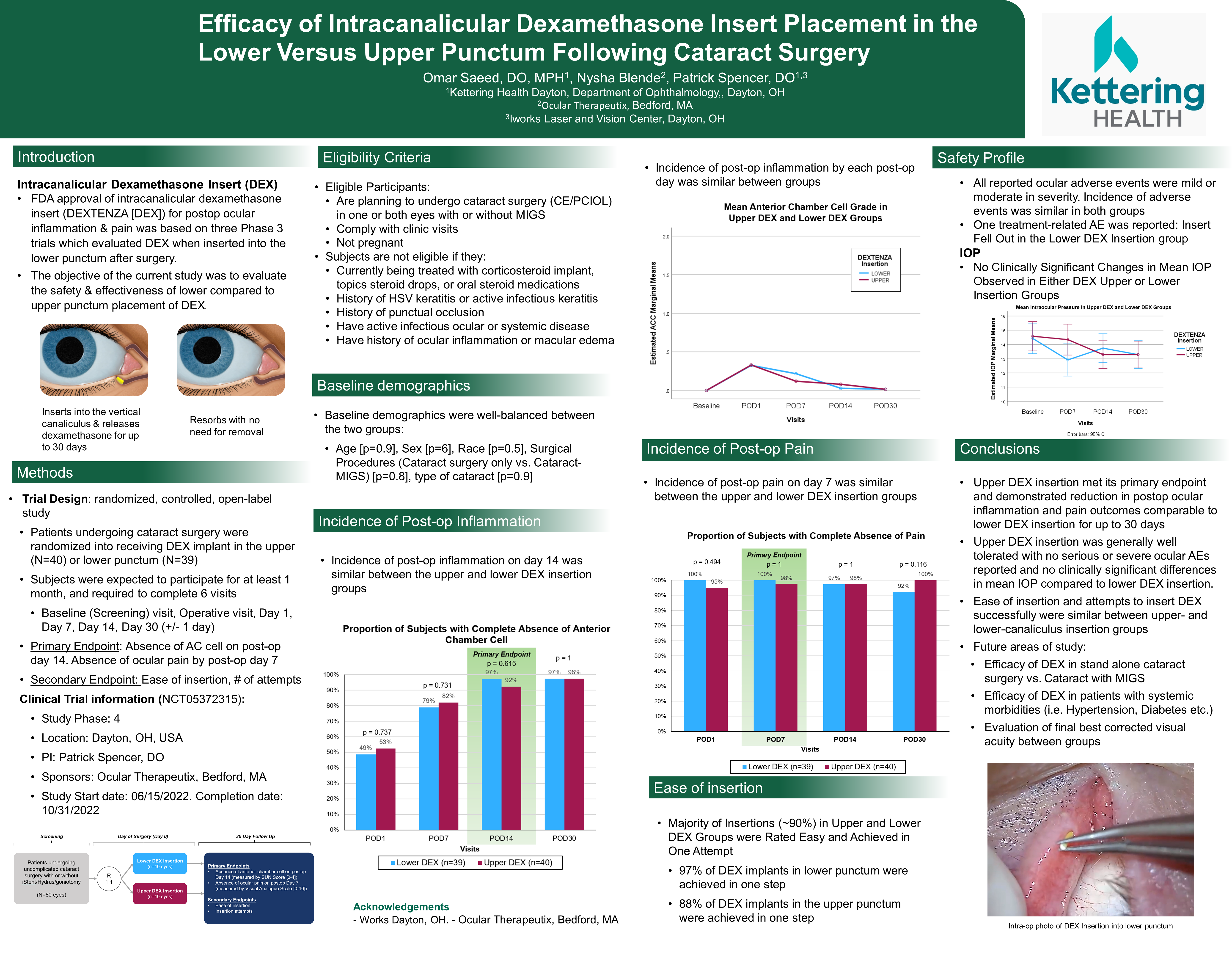
omar saeed DO
Efficacy of Intracanalicular Dexamethasone Insert Placement in the Lower Versus Upper Punctum Following Cataract Surgery
Omar is an ophthalmology resident at Kettering Health Dayton in Dayton, OH with a special interest in public health. His appreciation for ophthalmology stems from the comprehensive nature of the field, allowing for the full spectrum of prevention and management in diseases of the eye. His interest in public health stems from a deeper passion to promote human health through collaborative societal efforts while still maintaining an individualistic approach to medicine. This commitment to ophthalmology and public health has been reflected through his research projects which range from the implementation of novel glaucoma procedures to understanding the social influences of congenital facial anomalies. Omar hopes to integrate ophthalmology and public health in pursuit of a career in academia as a physician, educator and researcher.
Abstract
View Abstract
Summary
FDA approval of intracanalicular dexamethasone insert (DEXTENZA [DEX]) for postop ocular inflammation & pain was based on three Phase 3 trials which evaluated DEX when inserted into the lower punctum after surgery. The objective of the current study was to evaluate the safety & effectiveness of lower compared to upper punctum placement of DEX. Eyes undergoing cataract surgery were randomized to receive either DEX in the lower punctum (n=39) or upper punctum (n=40). Primary endpoints were absence of anterior chamber (AC) cell at Day 14 and absence of ocular pain at Day 7. Safety was assessed by adverse events (AEs) collection and IOP measurements. The proportion of subjects with absence of AC cell on day 14 showed no statistically significant difference between lower and upper eyes (97.4% vs 92.3% respectively; p =0.615). Absence of pain on day 7 showed no statistically significant difference between lower and upper eyes (100% vs 97.5% respectively; p=1.0). Additionally, there was no clinically significant changes in mean IOP observed in either DEX upper or lower insertion groups. Upper DEX insertion met its primary endpoint and demonstrated reduction in postop ocular inflammation and pain outcomes comparable to lower DEX insertion for up to 30 days. Upper DEX insertion was generally well tolerated with no serious or severe ocular AEs reported and no clinically significant differences in IOP compared to lower DEX insertion.